Background: A multi-system illness recently reported in recipients of the newest generation of metal-on-metal hip prostheses has been ascribed to toxic effects of cobalt and possibly chromium. Case Report: We present a case of insidiously developing neurologic illness that occurred in a physically active professional. Discussion: This case illustrates the potential for a hip prosthesis to occultly impair safe functioning of aviators. Based on this case and others, we suggest modifications to aeromedical policy relating to waiver requests after hip replacement, to include routine monitoring of serum cobalt and chromium levels in recipients of metal-on-metal hip prostheses. The evaluation of aviators having an elevated cobalt level is also discussed.
Through mid-2007, the US Air Force granted at least 20 waivers for aviators having hip replacements (6). To obtain such a waiver initially, the USAF requires a history, physical examination, and imaging, all largely directed to regional factors, i.e. periprosthetic structures and function. Similarly, civilian pilots with a prosthetic hip may fly unless they have restricted limb movement or significant pain (16).
Waiver adjudication based solely on regional factors is sensible if the only aeromedically significant complications of hip replacement are themselves regional. Until recently, this has been true. However, recent case reports in specialty journals from the United States and Australia refute this unstated assumption: they describe systemic disease arising from the newest generation of hip prostheses.
This systemic disease, termed "arthroprosthetic cobaltism," should be of special interest to flight surgeons because of its potential to be an obscure cause of impaired neuro-cognitive and sensory function.
The case presented here, an insidiously progressive multi-system disease after hip replacement, illustrates the potential of arthroprosthetic cobaltism to impair aviation performance for many months before clinical recognition. After summarizing the definition, genesis, and consequences of arthroprosthetic cobaltism, we conclude by suggesting changes in the waiver policy for selected hip prostheses.
Figure 1 is an expanded view of the case history (14), emphasizing the progressive neuro-cognitive and sensory impairments.
This 49 year old male surgeon and endurance cyclist received an ASR metal-on-metal right hip prosthesis (DuPuy, Warsaw, Indiana) after developing intractable osteoarthritis. He returned to full professional and athletic activity after the operation, but was never pain-free in the right hip.
His earliest non-hip symptoms occurred three months post-operatively. He became uncustomarily irritable, excitable and anxious. After exertion in hot humid conditions, painful geographic rashes were noted in the groin and axillae. He was able to maintain his usual level of professional and recreational productivity until 18 months post-implantation, when symptoms worsened, disability resulted, and he presented to medical care.
The illness included untoward mood, cognitive, and behavioral changes that were partially responsive to medication. Progressive pain and noise at the prosthetic hip, and multiple medical findings, were also noted (Figure 1).
Phenytoin was initially prescribed to stabilize mood and was replaced by lamotrigine. At 29 months, during a disabling depressive episode, bupropion was prescribed. A focal rest tremor that developed was initially ascribed to bupropion, but persisted after bupropion was discontinued. The tremor eventually resolved months after hip revision.
At 38 months a subtle right temporal superior quadrantopsia developed. Months later, a flashing light in the same quadrant, seen only during darkness, also developed.
The abrupt drops in work effort at 18 and 29 months were largely the result of mood dysfunction. The drops at 0 and 43 months were the expected post-operative recovery time.
Per Figure 1, serum metal ions were high when first checked 11 months post-operatively, and remained so until the metal-on-metal prosthesis was replaced by a ceramic-on-plastic revision at 43 months. The operative findings (14) included markedly elevated concentrations of cobalt and chromium in periprosthetic tissues and cerebrospinal fluid. Figure 2 shows a portion of the explanted prosthesis.
During the illness blood pressure never exceeded 140/90. Diastolic dysfunction, found at month 42 on a pre-revision echocardiogram, had not been present on the pre-ASR echocardiogram, and was noted to have resolved at 63 months (20 months post-explantation). Exercise tolerance, though improved at 66 months, has not fully recovered.
Progressive improvement in mood, cognition, confidence and creativity continues at 66 months. Therapy with lamotrigine and bupropion at low doses continues, in fear of relapsing depression. Relative fatigue persists, as do subtle visual field deficits. Comfortable professional productivity has returned to about two-thirds the pre-cobaltism level. The most recent ion levels, measured 53 months after the initial operation, were 1.2 mcg/l for cobalt and 7.5 mcg/l for chromium.
Medical conditions that impair neuro-cognitive, muscular, and/or sensory function typically add unacceptable risk to the aviation environment. Cobaltism has the potential to affect all of these functions.
Cobalt is an essential trace metal always present in human tissue; total body stores in a male adult are about 1 mg. Cobaltism is the pathological condition arising from excessive quantities of cobalt in tissue, blood, or cerebrospinal fluid. Largely bygone causes of cobaltism include industrial cobaltism (i.e. due to industrial exposure), epidemic alcoholic cobaltism (due to the one-time practice of adding cobalt to beer to improve the head), and iatrogenic cobaltism (due to the treatment of anemia with oral cobalt chloride).
The multiple clinical sequelae of cobaltism relate to its mitochondrial toxicity and have been known for 30 years. Classically, cobaltism presents with neurologic (central and peripheral), endocrine, and cardiac manifestations. Combinations of tinnitus, vertigo, deafness, visual impairment, electroencephalographic changes, weakness, muscle atrophy, paresthesias, hypothyroidism, and heart failure have been noted. Non-specific manifestations -- weight loss, headaches, irritability, fatigue and muscle atrophy -- are also frequently noted, and may be prodromal. Excessive dietary cobalt, in rabbits and rats, produces CNS depression and impaired learning. Direct application of cobalt-impregnated gelatin strips has been used to model epilepsy in rats, cats and monkeys (13).
When the source of the excessive cobalt is a prosthetic joint, the label "arthroprosthetic cobaltism" is warranted. It is reasonable to presume that the clinical consequences of cobalt excess depend on both the amount and the time course of cobalt exposure.
In recent years, approximately one-third of the 250,000 prosthetic hips implanted annually in the United States (1) have been "metal-on-metal" hips, i.e. both the ball and socket are made of a cobalt-chromium alloy. First implanted transiently in the 1960s and again in the 1990s, several manufacturers began offering a third generation of metal-on-metal hips 10-15 years ago, especially to younger patients, based on predictions of superior durability and toughness (4). The metal-on-metal hip bearing has been used in almost all recent hip resurfacing procedures.
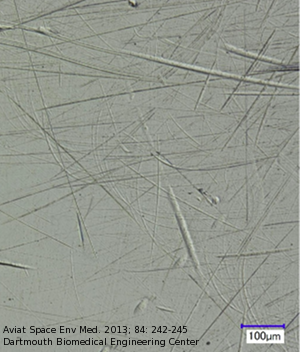
As with all prosthetic hips, wear and corrosion of the articulated metal-on-metal surfaces produces debris particles from these prostheses (Figure 2). Local accumulation of chromium-cobalt debris has been associated with multiple regional complications (7). One metal-on-metal hip, the "ASR" prosthesis, has been recalled due to hip pain arising from peri-prosthetic tissue damage caused by such debris (9).
Cobalt and chromium ions can elute from metallic debris particles, and so gain access to the systemic circulation (and distant body tissues). Systemic ion levels, therefore, parallel the peri-prosthetic burden of metal debris and are a marker for bearing performance (8). However, even in patients with a well-performing metal-on-metal prosthesis, the average cobalt and chromium ion levels exceed those in patients with metal-on-plastic hips (5).
Since October 2010, four cases of neurological arthroprosthetic cobaltism have been reported in patients having metal-on-metal hip prostheses (10) (14). Two additional cases, one of them surgeon-reported (2), are known. In five of these cases mood, memory, or “cognitive decline” were noted as early presenting symptoms.
Five severe cases of neurological arthroprosthetic cobaltism were reported before 2010, caused by ceramic debris wearing on chrome-cobalt prosthetic heads (3). In these cases profound blindness, deafness, or peripheral neuropathy preceded diagnosis. Seizures and overt heart failure, with arrhythmia, were also present in one case. Hypothyroidism was noted in four cases. The blood cobalt levels in these cases were 3-to-5-fold that of the case reported here.
Although chromium can affect mood (11), and rises in tandem with cobalt in patients with metal-on-metal hips, the neurological presentation in the arthroprosthetic cases has generally been attributed to cobalt because of similar presentations in classic cobaltism cases where chromium exposure was not present.
The inherent limitations of case reports are well known. As a recently-described illness of unknown prevalence, evidence-based guidelines cannot yet be formulated for arthroprosthetic cobaltism. To address these uncertainties, the US Food and Drug Administration recently ordered all manufacturers of metal-on-metal hip prostheses to conduct formal post-marketing studies of these joints, to determine the frequency and magnitude of systemic and periprosthetic complications related to metal-on-metal hips. The results of these FDA-mandated studies will likely not be available for years, but several characteristics of the disease compel attention by aeromedical specialists now.
First, the population at risk is large. Although aviators are usually younger than the typical recipient of hip prostheses, the metal-on-metal hips have been marketed especially for use in younger and more physically active patients (4). The older age among members of the military reserve components would also seem to be relevant.
Second, the insidious nature of arthroprosthetic cobaltism, with its non-specific symptoms and its ability to masquerade as simple hypertension or simple hypothyroidism or simple tinnitus, all but guarantees that cases will be diagnosed late, unless suspicion is always maintained at a high level. For example, our patient's hip symptoms were only activity-related and not limiting at the time when he was already experiencing neuro-cognitive, sensory, and muscular impairments that would have been unsafe in an aviation environment. Even at the time of revision surgery he maintained a higher level of hip function than he had before his hip replacement, despite extensive necrosis of his periprosthetic tissues. More worrisome, one reported case of arthroprosthetic neuro-cobaltism included a symptom-free hip prosthesis, unremarkable radiographs, and a serum cobalt level of just 15.5 mcg/l (10).
Arthroprosthetic cobaltism is easily and inexpensively ruled out by simple measurement of serum cobalt levels. The clinical experience to date has been that normal serum cobalt levels rule out cobaltism.
Unfortunately, an abnormally high cobalt level raises questions that cannot be answered in a rigorous, evidence-based way: What level, if any, rules in cobaltism? What level should prompt revision of the prosthesis? At what level should aviation duties be restricted? How should symptoms, signs, and imaging be weighted in these questions?
Typical of aerospace medicine, defining what is safe is always easier than defining what is unsafe. Ultimately, a flight surgeon who knows the whole patient well will have the best chance of making the correct judgment.
With these principles in mind, and motivated by prudence, we propose the following changes in waiver policy towards recipients of metal-on-metal prosthetic hips:
[1] All recipients of metal-on-metal prostheses should have at least annual measurement of serum cobalt and chromium levels, along with detailed questioning about hip function.
[2] If the hip is functioning well, flying duties should not be restricted if the serum concentration of cobalt is under 7 mcg/L as measured by inductively coupled mass spectrometry in a reference lab. (Rationale explained below.) Higher concentrations should prompt clinical and objective assessment for cobalt-associated pathology. (See Table I.)
| Parameter | Result(s) heightening concern |
|---|---|
| Regional Parameters | |
| Hip pain | More than minimal pain (consider CT/MRI) |
| Hip function | Less than "acceptable" |
| Hip x-ray (plain films, minimally) | Bone lysis near prosthesis (should prompt CT/MRI) |
| Cross-sectional imaging (CT/MRI) | Solid tumors or fluid collections near prosthesis |
| Systemic Parameters | |
| Blood pressure | Rise above baseline, even if normotensive |
| Exercise tolerance | Decrease from baseline |
| Visual acuity | Decreased and non-correctable vs. baseline |
| Visual fields | Any abnormality |
| Audiogram | Decrease from baseline, especially in high frequencies |
| Thyroid function tests | Hypothyroidism or "euthyroid sick" |
| Mood | Change from baseline, up or down |
| Cognition and memory | Decrease from baseline |
[3] In aviators having well-functioning metal-on-metal hip prostheses and low serum metal levels, consider baseline assessment of the systemic parameters in Table I.
[4] Military and civilian authorities should study and develop evidence-based standards for assessing recipients of metal-on-metal implants. At a minimum, all future waiver requests for prosthetic hips should disclose what type of prosthesis was implanted.
[5] Any decision to revise a metal-on-metal hip should be made by the patient and his or her orthopedic surgeon, with the flight surgeon providing input on occupational ramifications.
[6] Aviators considering hip replacement should, despite the sparse data, be informed of the potential for arthroprosthetic cobaltism and the possible effect on their careers.
More detailed recommendations for the follow-up and management of metal-on-metal hip recipients exist (15), but they are based on a very small number of cases.
The recommendation to allow flying duties for serum cobalt levels below 7 mcg/l is necessarily ad hoc. It is the same threshold set by British healthcare regulators as indicative of metal-on-metal hip bearing that requires further evaluation for periprosthetic tissue damage (12), and is half the lowest value associated with a case of neurologic arthroprosthetic cobaltism (10). A case without neurological involvement despite a cobalt level of 90 mcg/l (3) illustrates that the toxic threshold may vary significantly between individuals. Idiosyncrasies of cobalt's protein binding and membrane transport have been suggested to contribute to the variability (3).
As in all insidious multi-system diseases, however, a high index of suspicion is the flight surgeon's best ally.